What is a Do Not Resuscitate (DNR) order in Wisconsin?
A Do Not Resuscitate (DNR) order in Wisconsin is a legal document that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if a person's breathing stops or if their heart stops beating. It's intended for use by patients with a serious illness or condition where CPR would not be expected to significantly extend their life or improve their quality of life.
Who can request a DNR order in Wisconsin?
In Wisconsin, a DNR order can be requested by any adult who is of sound mind or by the legal guardian of a person who is not able to make such decisions for themselves. Additionally, healthcare agents appointed through a valid durable power of attorney for healthcare may also request a DNR order on behalf of the person they represent.
How can someone obtain a DNR order in Wisconsin?
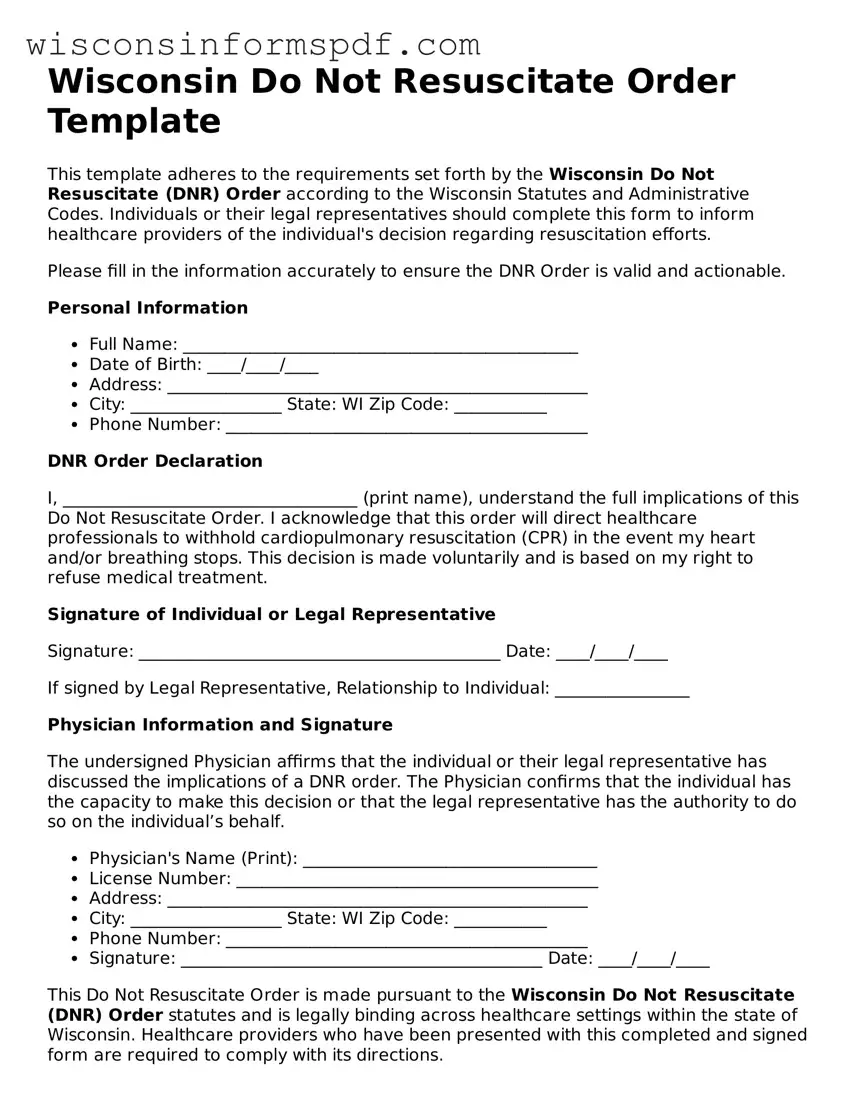
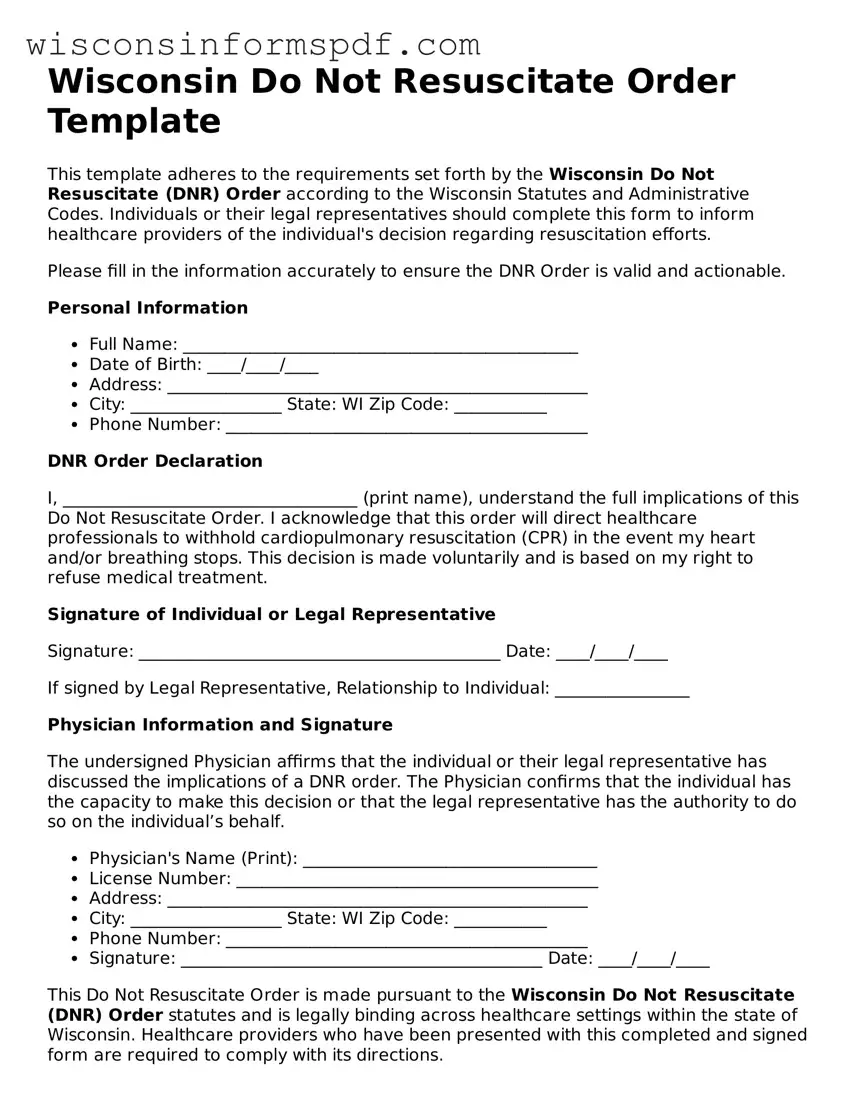
To obtain a DNR order in Wisconsin, the individual or their authorized representative must first discuss their wishes with a licensed physician, advanced practice nurse practitioner, or physician assistant. If a DNR order is deemed appropriate, the healthcare provider will fill out the official state form, which must then be signed by both the healthcare provider and the patient or their representative.
Is the Wisconsin DNR order applicable in all settings?
Yes, the Wisconsin DNR order is applicable in all settings, including the patient's home, in a hospital, or in other healthcare facilities such as nursing homes. It is designed to ensure that the patient's wishes regarding CPR are respected across all settings.
What should someone do with their DNR order once it's obtained?
Once a DNR order has been obtained, it is advisable to keep it in a location where it is easily accessible to emergency personnel. Copies should be provided to family members, healthcare agents, primary care physicians, and the main hospital or healthcare facility where the person receives treatment. Some people also choose to wear a Wisconsin Department of Health Services-approved DNR bracelet to indicate their DNR status.
Can a DNR order be revoked or changed in Wisconsin?
Yes, a DNR order can be revoked or changed at any time by the patient or their appointed healthcare agent. To revoke a DNR order, the individual must inform their healthcare provider verbally or in writing. A new DNR order can be issued if the person's healthcare wishes change and they no longer wish to have a DNR status.
What is the difference between a DNR order and a living will in Wisconsin?
A DNR order specifically relates to the refusal of CPR in the event that a person’s breathing or heartbeat stops. A living will, on the other hand, is a broader document that outlines a person’s preferences for various types of medical treatment and interventions in the event they become incapacitated and cannot express their wishes themselves. While both are advance directives, they serve different purposes.
Is there a fee to obtain a DNR order in Wisconsin?
There is no fee to obtain the DNR order itself in Wisconsin. However, there may be costs associated with consulting healthcare providers to discuss and complete the DNR order form. Additionally, if someone chooses to purchase a Wisconsin Department of Health Services-approved DNR bracelet, there may be a cost for the bracelet.